Couples (Relationship) Therapy

Couple therapy is a type of therapy which involves a couple and a therapist. While the couple works on their relationship, the therapist creates an environment that enables change in the couple's relationship.
The primary aims of couple therapy are to enable the couple to:
- identify unhelpful relational patterns in the relationship
- understand the source of reactive emotions that drive the pattern
- utilize their acquired skills in managing or resolving their problems
- establish strategies for maintaining healthy relationship
- improve their communication by expanding and re-organizing their emotional responses in the relationship
- hear the other and be heard
- contribute to the decisions regarding their relationship
- foster a secure attachment between partners.
- maintain a sense of intimacy.
Couple Therapy Principles
Our couple therapy is based on the core principles of:
- Respect
- Empathy
- Tact
- Consent
- Confidentiality
- Accountability
Though our couple therapy involves the couple and therapist, there are occasions where the couple will be seen apart. This is done if the therapist perceives that the couple may be having personal issues which they may consider as controversial, shameful or difficult to share with spouse. The issues discussed during such sessions are considered as confidential, hence, will only be discussed in the couple therapy except the spouse raises them.
Common problems:
The following are some of the common (but not exhaustive) presenting problems that couples are faced in their relationships:
- Communication difficulties
- Loveless Relationship
- Toxic Relationship
- Extra-marital affairs and broken trust
- Stress and anxiety relating to divorce/separation
- Step-family difficulties
- In-laws and/or extended family difficulties
- Domestic violence.
- Culture clash in inter-racial relationship
- Attachment issues (e.g. unresolved childhood issues, repeat negative patterns in relationship, rejection, abandonment, possessiveness, non-committal relationship)
- Sexual and Reproductive issues in women and men etc.
Sexual and Reproductive Issues
In our therapeutic work with men and women with sexual and reproductive issues, we sometimes collaborate with medical teams (NHS and private) to develop our care plan for our clients. We offer therapy to clients with the following challenges:
WOMEN ISSUES
- Low sex drive (libido)
- Dyspareunia
- Menopausal issues
- Unplanned pregnancy
- Infertility/sub-fertility
- Contraception and Post-termination of pregnancy
- Recurrent miscarriages, Still births, Abnormality/disabilities
- Poly-cystic Ovaries, Endometriosis, Fibroid etc
- Post-Natal Depression (PND)
- Post-Natal Body Dysmorphias
MEN ISSUES
- Sexual Dysfunction (no erection, early ejaculation)
- Infertility/sub-fertility
- Mid-age crisis('Manopause')
- Low or excessive libido (sex drive)
- De-masculinised self-image
- Attachment and role-model issues
If you and/or your partner are experiencing any of these problems listed or others not listed, please contact us and we we will book you into the nearest available time. Our appointment booking time is within 3 - 5 working days.
DYSPAREUNIA: PAINFUL INTERCOURSE
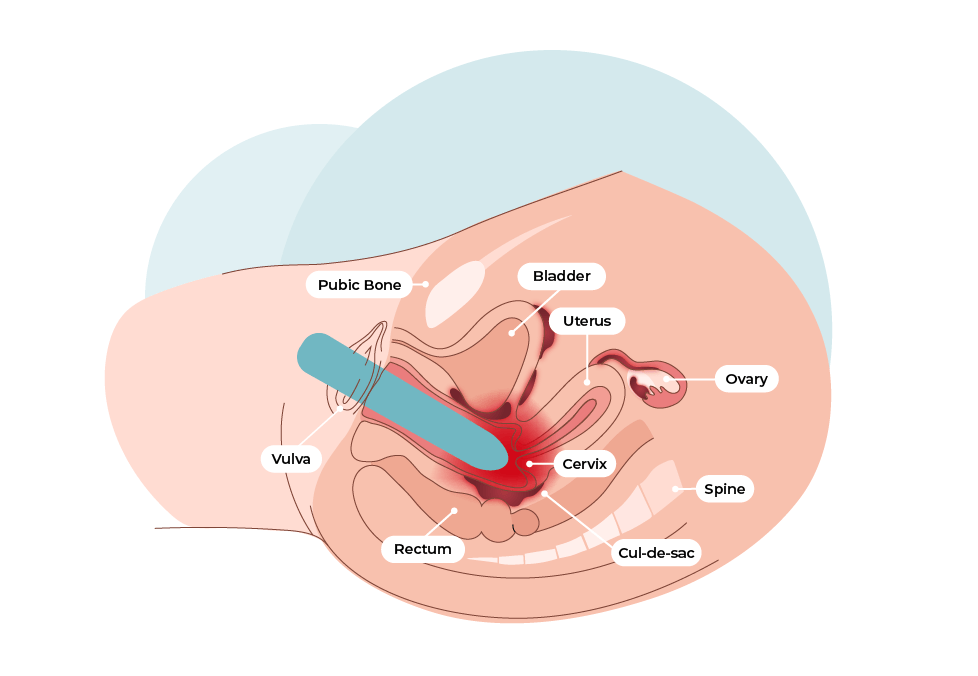
DYSPAREUNIA (PAINFUL INTERCOURSE)
Overview
Dyspareunia is described as persistent or recurrent genital pain that occurs just before, during or after intercourse.
Symptoms
The following are the common symptoms of painful intercourse:
- Pain only at sexual entry (penetration)
- Pain with every penetration, including putting in a tampon
- Deep pain during thrusting
- Burning pain or aching pain
- Throbbing pain, lasting hours after intercourse
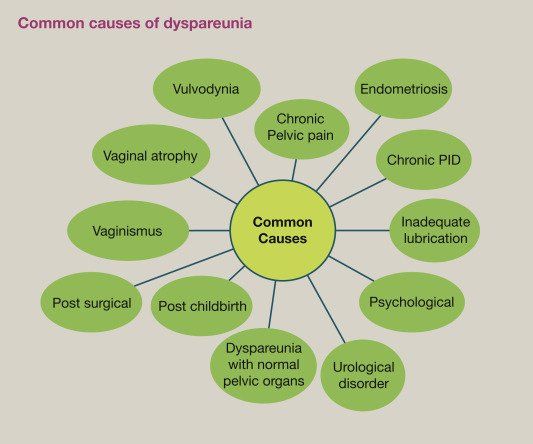
Causes
- Physical causes of painful intercourse differ, depending on whether the pain occurs
- at entry or
- with deep thrusting.
- Emotional factors might be associated with many types of painful intercourse.
Physical causes: Entry pain
Pain during penetration might be associated with a range of factors, including:
- Lack of experience by the couple
- Not enough lubrication.
- This is often the result of not enough foreplay.
- A drop in estrogen levels after menopause or childbirth or during breast-feeding also can be a cause.
- Certain medications are known to affect sexual desire or arousal, which can decrease lubrication and make sex painful. These include
- Antidepressants,
- High blood pressure medications,
- Sedatives,
- Antihistamines and
- Some birth control pills.
- Injury, trauma or irritation. This includes:
- Injury or irritation from an accident,
- Pelvic surgery,
- Female circumcision or
- Episiotomy (cut made during childbirth to enlarge the birth canal).
- Inflammation, infection or skin disorder.
- An infection in your genital area or urinary tract can cause painful intercourse.
- Eczema or other skin problems in your genital area also can be the problem.
- Vaginismus. These involuntary spasms of the muscles of the vaginal wall can make penetration painful.
- Congenital abnormality.
- A problem present at birth, such as the absence of a fully formed vagina (vaginal agenesis) or
- development of a membrane that blocks the vaginal opening (imperforate hymen), could cause dyspareunia.
Physical Causes: Deep pain
Deep pain usually occurs with deep penetration. It might be worse in certain positions. Causes include:
- Certain illnesses and conditions. The list includes:
- Endometriosis,
- Pelvic inflammatory disease,
- Uterine prolapse,
- Retroverted uterus,
- Uterine fibroids,
- Cystitis,
- Irritable bowel syndrome,
- Pelvic floor dysfunction,
- Adenomyosis,
- Hemorrhoids
- Ovarian cysts.
- Surgeries or medical treatments.
- Scarring from pelvic surgery, including hysterectomy, can cause painful intercourse.
- Medical treatments for cancer, such as radiation and chemotherapy, can cause changes that make sex painful.
Emotional Factors
Emotions are deeply intertwined with sexual activity, so they might play a role in sexual pain. Emotional factors include:
- Psychological issues.
- Anxiety,
- Depression,
- Body Dysmorphia (concerns about your physical appearance)
- Fear of intimacy or
- Relationship problems can contribute to a low level of arousal and a resulting discomfort or pain.
- Stress. Your pelvic floor muscles tend to tighten in response to stress in your life. This can contribute to pain during intercourse.
- History of sexual abuse. Not everyone with dyspareunia has a history of sexual abuse, but sexual abuse can play a role.
- Initial pain can lead to fear of recurring pain, making it difficult to relax, which can lead to more pain.
Diagnosis
A medical evaluation for dyspareunia usually consists of:
- A thorough medical history. Your doctor might ask when your pain began, where it hurts, how it feels and if it happens with every sexual partner and every sexual position. Your doctor might also inquire about your sexual history, surgical history and childbirth.
- Providing accurate information to your doctor is very crucial. Do not let embarrassment stop you from answering truthfully. These questions provide clues to the cause of your pain.
- A pelvic exam. During a pelvic exam, your doctor can check for signs of skin irritation, infection or anatomical problems. He or she might also try to locate your pain by applying gentle pressure to your genitals and pelvic muscles.
- A visual exam of your vagina, using an instrument called a speculum to separate the vaginal walls, might be performed as well. Some women who have painful intercourse also have discomfort during a pelvic exam. You can ask to stop the exam if it's too painful.
- Other tests. If your doctor suspects certain causes of painful intercourse, he or she might also recommend a pelvic ultrasound.
Treatment
Treatment options vary depending on the cause of the pain.
Medications
- If an infection or medical condition contributes to your pain, treating the cause might resolve your problem.
- Changing medications known to cause lubrication problems also might eliminate your symptoms.
- For many postmenopausal women, dyspareunia is caused by inadequate lubrication resulting from low estrogen levels. Often, this can be treated with topical estrogen applied directly to the vagina.
Drug: Your doctor may prescribe medications such as:
- Ospemifene to treat moderate to severe dyspareunia in women who have problems with vaginal lubrication. Ospemifene acts like estrogen on the vaginal lining.
- Prasterone. It's a capsule you place inside the vagina daily.
Therapy
Non-medication therapies also might help with dyspareunia:
- Desensitization therapy. You learn vaginal relaxation exercises that can decrease pain.
- Psychoeducation. If sex has been painful for some time, you might have a negative emotional response to sexual stimulation even after treatment. If you and your partner have avoided intimacy because of painful intercourse, you might also need help improving communication with your partner and restoring sexual intimacy. Talking to your therapist can help resolve these issues.
- Cognitive Behavioural therapy also can be helpful in changing negative thought patterns and behaviours.
- Sexual practice experience
You and your partner might be able to minimize pain with a few changes to your sexual routine:
- Change positions. If you have sharp pain during thrusting, try different positions, such as being on top. In this position, you might be able to regulate penetration to a depth that feels good to you.
- Communicate. Talk about what feels good and what does not. If you need your partner to go slow, say so.
- Do not rush. Longer foreplay can help stimulate your natural lubrication. You might reduce pain by delaying penetration until you feel fully aroused.
- Use lubricants. A personal lubricant can make sex more comfortable. Try different brands until you find one you like.
- Please contact us at FCC Clinics if you are your partner is experiencing dyspareunia




